Health system interim report - Our response
From Dr Brendon Eade, Pinnacle Incorporated Deputy Chair
The broader Pinnacle Group sees the Health and Disability System Review - Interim Report as effectively highlighting many of the key challenges and opportunities the New Zealand health sector is facing.
On some levels the system performs well, but needs future proofing to ensure it is resilient and fit for purpose. For this to be enabled many of the issues identified need to be effectively addressed with a commitment to action.
For Māori in particular, and for high need populations, a shift from hospital-based care to more culturally appropriate community and closer to home settings will need to be a key feature of the future sector.
If we are to truly realise the system change required, a stronger and more purposeful leadership is required across the system. The recent period of risk management and containment has not served New Zealand well, leaving many gaps and failing services in primary care as leadership has failed to challenge the performance and the behaviour of the system.
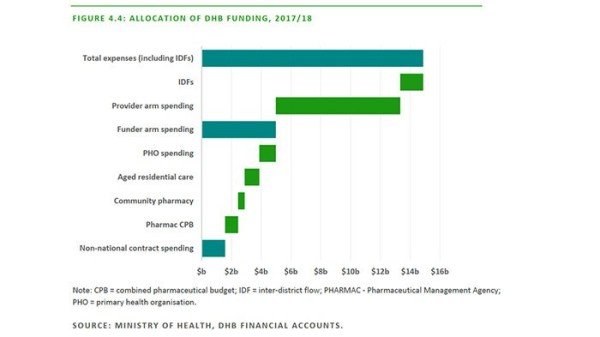
The following figure in the review points to the core challenge the sector faces with $10b going into hospital care that has high fixed labour costs, what appears to be low productivity and for care that could have been prevented with a higher investment in primary care services.
Primary and community care total spend is a tiny portion of the total funding and the impact is reflected throughout the document through Māori, Tier 1, Disability and many of the enablers around access, cost, data and capacity.
The review is highly disappointing in its deficit view of primary care and lack of acknowledgement or understanding of the significant proportion of New Zealand healthcare it delivers with disproportionate funding. This is exacerbated with the increased investment going into hospitals. It could be cynically argued this is reflective of the current government's politics; a mirror of the original labour primary care strategy. The few examples offered are small unscalable examples rather than the broader system focused shifts that have occurred.
While articulating strongly for a shift of focus and integration of services in a community setting the review mostly covers DHBs and their governance arrangements and remains largely silent and uncommitted to how the refocus would occur.
The explicit reference to the Regional Midlands Health Network Charitable Trust PHO and intimation that is was a 'shell entity' does a real disservice to the community representatives, iwi, Māori health providers and health professionals on the PHO Board who meet regularly to lead, monitor and shape the work of the PHO and the broader Pinnacle Group.
This configuration came about when five PHOs were consolidated across the midland region under stronger iwi, community and provider governance. Rather than building more entities and wasting public funding on reconfigurations the PHO has leveraged off collective arrangements.
It also more importantly ignores how effective this configuration has been, as part of the Pinnacle Group, that has pioneered a wide range of projects that have and continue to have both national and international impact.
- Health Care Home (independently evaluated as having most impact on Māori and socially deprived populations and now being rolled out nationally).
- indici, the first cloud based patient health and well-being platform for the future that empowers patients to control their own health and wellness information including genomics, that is also being adopted nationally and internationally.
- Pioneered the first general practice based Māori community health workers now being adopted across the regions together with the first practices to embed Māori whānau and group consultations, also now being adopted by others.
- Development of the first national primary and community care data sets within public cloud settings that are playing a huge role in supporting new models of care and system planning.
- A a social enterprise alternative to corporate ownership for primary care services especially in high need rural communities where the low returns fail to attract the alternatives.
Overall the 'interim' report, whilst highlighting key issues facing healthcare in Aotearoa probably has missed the opportunity to engage New Zealanders in a sensible discussion about what the art of the possible might be.